For Nkechika, all residents of Delta must have access to quality health care as such, health care must be accessible and affordable to all.
In this interview where The Story, was present, the Director General, the Delta State Contributory Health Commission, spoke about the success stories of the Commission and the efforts put in place to making sure that Primary Health Centres are equipped for rural dwellers.
Excerpts:
What Is the Delta State Contributory Health Commission All About?
The Commission was borne out of a situation in the country where the country realized that 97 percent of residents of Nigeria were paying what we call out of pocket. So, when you are sick, you go to the hospital. You pay for card, consultation, drugs, lab, and you pay for everything.
So, by the time you go through that, one’s time is wasted, you have to pay cash for everything and it now turned out that a lot of people that are poor and not indigents, when they are now sick, they have two options, they either go and borrow money putting them into more poverty or they go to native medication which worsen their health or they just live life like that.
It became a problem where it was noticed that if they start up a programme where there is a collective effort towards health care financing, that somewhere along the line, there will be a balancing factor. That ability also puts health on the front burner where hospitals are now properly equipped to operate and then people are now able to work into the hospitals even when they don’t have money to provide care and that is basically what they call health insurance.
Just like vehicle insurance and co. So, it was determined that there should be health insurance in the whole country and that is how NHIS was birthed. And after several years, they realized that NHIS at the national level was not spreading well, just remaining in the urban areas. So, in 2015, they now passed a new resolution that NHIS should decentralized to state. So, state will now setup what they call state supported health insurance programme because in that way it takes this same thing down to the grassroot. So, somewhere along the line when the current governor of Delta state, Dr. Ifeanyi Okowa, was chairman, Senate Committee on health, he was spearheading this health insurance programme and I was actually doing a course abroad and we happen to meet and had common interest. So, we started developing the policy to implement it in Delta State and as soon as he became the governor, infact while he was campaigning I was actually doing the blueprint and as soon as he became governor, the bill was ready.
We presented it to him, he took it to the house of Assembly and I thought my job was over and I travelled back to Abuja and they called me back that what you have done you have to come and implement it. That is how I found myself to getting this job done to ensure that all residents of Delta State have access to quality health care irrespective of their socio economic status and geographical location. And in it there is a form which has been provided, where all poor people, pregnant women, children under five, elderly above 65, physically and mentally challenged will be able to go to a hospital to receive care even if they don’t have money and the hospitals will be able to provide them.
Now, one critical thing, the way it is done is that health care was now split into two: there is what we called demand for healthcare then supply of healthcare. So, the health insurance demands for healthcare on behalf of the populace while the ministry of health supplies healthcare service on behalf of the doctors. So, we meet at a junction where if you provide quality healthcare for the people, we pay, that is basically how we came about this whole process to correct this imbalance in access to healthcare between the rich and the poor and people living in the rural communities and people living in the urban communities.
The key point is to avoid a situation where people have to pay to receive basic healthcare. Now, one critical thing is that insurance cannot take care of everything but what we did is that we design it in such a way that 50 percent of the disease burden in Delta state was properly captured. Like when we started we had meetings with Okada riders, market women, farmers, fishermen. Everybody come and tell us what is your most challenging health situation and that was how we developed what we called the benefit package. Initially when it was done, it was supposed to be N17, 000 a year per person but when we did an analysis we realized that for the average family in Delta state to pay N17, 000 for each individual was a problem so we approached the governor he now reduced it to N7, 000 but also we now find ways to cushion it, so that it is sustainable to government. That is why you see that the premium is N7, 000 but what we are providing is N17, 000 per person and surprisingly it has been adopted across the country.
At A Time When The Issue Of Deduction From Husband And Wife In The Civil Service Came Up, How Was It Handled?
The first thing is that when we started, there is a payroll in Delta state where Biometric data was collected by Heckerbella. So, instead of going to civil servants one by one, they gave us that data. We uploaded it from day one. So, every civil servants was registered in one day but because the data they collected was employment data, health care service data is very peculiar. People would have had a wrong age, you know age is very important in the quality of medicine that they give to you. We now said that though we have collected your data but you need to come and look through what we have and confirm that what is there is correct so that when it is correct we now print your ID Card and give to you.
That is the first thing we did. We also said that if more than one member of the family is earning, they will choose who will become the principal person then every other person is recorded as dependant. If you look at our ID Card, you will see DEP. It means dependant. So, there is only one principal in the family, all the others will not pay. Even in our law if the husband is contributing from NHIS, the entire family is exempted. So, even a civil servant here that the husband is in the NHIS scheme, the wife does not need to collect that is even when you are a civil servant on the state and it is properly documented.
But because we are just a beneficiary, all they do at the end of every month is that they will send us that these are the people whom they deducted money from for the month. So, we setup a system it was even sent as circular that all civil servants should write through their MDAs to head of service so that they stop their deductions from payroll because the deduction is done at payroll monthly and we have copies so when you send we have copy but you know because is manual, when they give you the list it is difficult to start checking.
So when you complain officially to us, we will tell you go to head of civil service, deduct it from payroll because we cannot utter the payroll because our law is very clear, only one member of the family is deducted and even if a member of the family has a husband or a wife that is in the federal NHIS, you are exempted in Delta state, they don’t collect from you that is the standard here. So, we don’t control it, we just receive data and we just have A, B and C. So, that’s the process, but we are not involved in it, we just collect data and what is given to us at the end of every month.
Most Civil Servants In The State Complained That When They Visit Hospitals, They Are Not Attended To As Expected And Many At Times, They Are Just Given Only Paracetamol, What Is Your Commission Doing About This?
Yes! We have received such complaints and we put in certain measures so we first of all look at our operational guidelines. There is a penalty. So, if you go to a hospital, you either don’t receive care or they don’t receive care on time, they don’t receive the appropriate drugs or does not even get treated well. First of all that hospital would be fined N200, 000, it is gazetted, the head of the hospital will be penalized. In fact, we have made it so serious that if it is a doctor, we report to Nigeria Medical and Dental Council. If it is a nurse, we report to Nurses Council.
At a higher level, we can actually report to the Attorney General, the person can actually be prosecuted and the person can become an ex-convict with a fine. But the question is this, you cannot go through that level accept you have hard copy evidence. So, what we did when we noticed that initially was to put what we call suggestion boxes in every hospital so that if you have complaints, write and put it there.
We realized that when we go to the suggestion boxes, somebody will break it and take them away, we now put in what we called agents, we have our agents, we call them mystery patients. Sometimes, we send mystery patients to go and check, we have them in the hospitals walking around and we actually have reports of workers but all we can do, is write a report.
We cannot prosecute because for us to be able to do that, there must be a panel setup by the supply side. The Ministry of Health has the mandate, we cannot summon a doctor or a nurse for not attending to someone. So we write to the Ministry of Health, they investigate and take action. But on our own we won’t let that continue. If you look at the back of every card, there is a number there, a 24hr number. So we told all our enrollees, if you are in a hospital and you are having challenges just dial that number. I was even the person that has that number for sometime until it became very overwhelming for me so I decided to assigned a staff and we increased the number to four, two of the phones are among that list and it is always with me.
I carry it everywhere, the reason I do that is just in case anybody start calling this number that means all my other staff are not answering their own. But the problem is if we get the call, what we can do is to call the hospital. Infact, one honourable member called me three weeks ago that he is in a hospital and they asked him to pay N3,000 and I said fine, you are an honourable member, pay collect and evidence of the receipt, I will personally refund your money. There is also a case that we are investigating but even in the investigation we have to be careful to protect it.
A woman went to a lawyer to borrow N20, 000, she said she went to a hospital to give birth and that they say she should bring N20, 000, and I said give to the woman let the woman give to the doctor and get me the information. Let him finish treatment that doctor is in trouble because we have been able to track that information but the question is how many can you trace? That is why we setup that programme where if you are having any problem at the point of care, you call but we we also try to talk to the Ministry of Health. What we now further did was that we setup the labour monitoring committee, NLC is part of it, nursing council is part of it, TUC, is part of it, NMA is part of it. All Labour union setup a committee, once we see such cases we follow it up.
While we are following it up in the technical way, we are also following it up the labour way so that even when we apply sanction, labour will not jump at us that why are you doing that. All in an effort to correct that situation. It is an insurance, you are supposed to provide primary care first. So we do a lot of advocacy to educate the doctors and the nurses that look at the situation. Infact, there is what we called the benefit package, that is pasted in every hospital because it is not all cases that are covered. Sometimes people go to the hospitals they are told this is not covered and we tell them to point at it or we tell them to call us. We tell the patient either yes, this is covered or is not covered or we tell the doctor this is covered or is not covered.
But one thing we also do, any patient who comes to the hospital, whatever situation the patient has you must provide the care because we have that provision for the patient. If a woman comes to the hospital and she is in a medical condition, you won’t say because it is not covered, the woman should die, no. Provide care, we know how to handle those extras but also to prevent abuse that is why that restriction is put in place. So, yes it exist, we investigate, there are sanctions, we have penalized certain people but what will help us is educating the people, letting them know that at the back of your card, there is a number there. If you are having any problem call that number, if you are told to do this bring the evidence, we will prosecute the people, that is the best we can do but we will continue to strive on, but the most important thing is that education. Educating people that it your right. You know what people don’t understand, in the previous system, you are buying healthcare but in health insurance, you have paid upfront. So, your rights are even stronger. So, once you pay health insurance, it is a malpractice for the hospital not to be opened.
If a hospital changes its address without informing us, you are sanctioned because you must remain open for the enrollees that you have received payment for. So, if you have collected somebody’s money, you must provide care, you must be available, you must treat the person on time. We are taking it to the next level, to what we call patient rights. Let the patients know their rights and let them know that you can actually make a case and succeed in it. We are empowered to act, we need information and we need supporting action.
Since The Inception Of Governor Ifeanyi Okowa Led Administration, We No Longer Hear Of The Free Under 5 And Maternal Care For Pregnant Women Put In Place By The Former Governor Emmanuel Uduaghan Led Administration, What Happened?
When we were designing the programme, infact, we were happy that such a programme was existing that there was this free under 5 and maternal. Actually that was what we started with. On 1st of January 2017, we started by following that programme. It is existing everyday but there was a difference. When we started those services were only in government hospitals that were in town and we noticed that a woman will drive an SUV, drive into an hospital and receive free treatment.
Meanwhile, in the rural communities where these poor people are, it was not available. Infact, we found one situation where one taxi driver, will park at the bridge head, carry pregnant woman, cross the bridge drive into Okwe, receive free treatment, collect medical bills from them and drive them back. So, we now said the programme will continue but it will go to primary healthcare centres. Not only in the urban centres because it was only in the general hospitals. It should also go to the rural communities, so we started with 100 PHCs to add to the existing ones.
The programme continued but it expanded. Two, we realized that we need the data because looking at such a beautiful programme for eight years, no records. Let say throughout that programme, there were 1000 pregnant women. How many survived? How many went through CS? What is the data? How many were children? Who followed them up? If you don’t collate that data and you know data is keen. Information is money so that was why we started to make sure that every pregnant woman that walked into the hospital, we collect your name, age, sex, LMP for both your husband and your children so that we take that family as a treatment unit as against just treating the mother.
So you find a situation where the mother has come for treatment, you have treated the mother, the child has come for treatment, you have treated the child. Meanwhile, there might be a disease condition linking the two, you won’t know. So, when we register the mother, we register both you and all the children in the family. Yes, we are providing free healthcare for the under 5 and the pregnant mother because we also watch where the family is, we tell them bring your husband. So we started collecting data. As at last records its over 6000 pregnant women and children under 5 that we have treated under this programme.
We are the only state in the country that has received that award from the world bank under it you save a million lives. That Delta is the state where you have the highest number for the poor and vulnerable population. If we are not doing it we will not receive these awards. Since 2017 till date, we are still maintaining that number one position. Nobody has challenged us and what we are saying is that this information is verifiable. If you want to know how many pregnant women we have delivered, their names, pictures, you will see all there.
We transitioned it. The difference is that we are now collecting data and we now spread it to primary healthcare centres. One other thing too is that when we started this health insurance scheme programme, we didn’t want it to be a political propaganda, we wanted our service to speak for us and not the jingles to speak for us. So, for the first few years, we were concentrating on building a structure and we are working hard. There is basically no community in the state that I have not been to. Why? Because we go there to check, to monitor. If you go to most of our hospitals, we have what we call community based agents.
They go from house to house in every community, letting them know that every child under 5 in the community, if you go to the hospital don’t pay, if they tell you to pay call us and these people are residents of the communities. So if a woman goes to the hospital and they tell you to pay just call them and they all have a handset. They also tell them how to live well. So, we are doing what we call house-to-house education. We had a meeting with President Generals of all communities, all the traditional rulers in Delta state, it was the same message we said they should pass on.
So, we have done it in several levels until we now realized that the most effective one is this house-to-house. So every day our agents post to us the number of house they visited. We are not doing the propaganda in town we are doing it in the rural communities because if you keep doing health insurance in the town, the poor people are actually in the villages, they are the people that actually need it that is why we took the service there. Like the first time I came, we couldn’t find one viable facility in the villages but today we have one in Porogbobo, for the Egbema and Oporoza for Gbaramatu kingdoms. We have setup for the Ode-Itsekiri, for the Itsekiri kingdom, we are starting Irri for the Isoko area. Why are we doing that?
To make sure that healthcare services are available to people. Our strategy is that nobody should travel more than 30 mins to receive health care, it should be a walking distance for you to get healthcare services. So, we are not the publicity type, we believe that our work will speak for us.
What Efforts Have You Put In Place To Replicate The Urban Success Story Of The Scheme In The Riverine Areas?
When we first started, we visited all the facilities in Delta state. There were 420 PHCs in our database, very few of them met the minimum standard for a health insurance scheme. When we saw that in the LGAs, they have a large landmass, we increased it to 110, we later moved it to 200 as I am talking with you, we are starting off a 300 PHCs across the state. Infact, I have sent two teams, the first team went to do an assessment.
Our mandate is to accredit only hospitals that are qualified but we realized that if we do that a lot of people will suffer that is why we are now going the extra mile of supporting the facilities to become acredited. We have provided the MTN solar lights for the 300 healthcare centres and the health insurance has been paying for it for the past two years, the very day that light go off, you call us and we intervene. Recently, we have been able to provide them with ICT, all the nurses now have a phone were they can call us directly because we have about three doctors working there.
They can call us if they have any medical situation that they need an intervention and any challenges of any type and we developed a software, if a patient walked into any PHCs in the village, all the nurse need to do is to type in the sickness that the patient says he or she has, it will guide the nurse to form a diagnosis, on the type of drugs to prescribe, on the type of laboratory test to do, if it is possible to do test but the bottom line is that it will guide the nurse to make sure that he sustains that life and if the nurse now sees that it is a serious condition, she calls. Because it is a CUJ line, we have paid.
So a doctor can call you and speak with you for over two to three hours and guide you on how to look after the patient pending when we rather send a doctor there or they evacuate the patient to further attention and treatment. This system is available in 300 PHCs that I am talking about. For security, we realized that one of the reasons too some personnel don’t stay in their hospitals, is because there is no security, we encourage them to make sure that they have a relationship with the vigilante in the community. In my village it cost just N10, 000.
The biggest issue was drugs because most of them were not getting drugs. We had a relationship with Drug Revolving Fund to supply the PHCs with drugs, they said sometimes they don’t pay and we said if they don’t pay come to us we will pay you, we guarantee that but the most critical thing which was affecting it was this. They see patients but they don’t see the money of the patients they see. So, under the health insurance scheme, every PHC that sees patient, they send the bill to us and we pay it back directly to the PHC. The nurse in charge is the signatory to the account. Not Ministry of Health or agency.
The account is opened in the name of the PHC, the money is paid directly into the PHC, the nurse is responsible with the expenditure. Look at what they do with the money, they can actually employ ad-hoc staff and pay, they can use that money to repair the hospital, they can get their allowance, if you have a generator, you can use that to buy fuel. Just record it. From the records I have, we have paid over N200 million to PHCs directly because it is the nurse in the hospital that knows what the hospital needs. We call those ones our star clinics because we do what we call a hub and spoke phenomena because there are certain things PHCs cannot do. What we have done is that we have selected some strategic hospitals where surgery can be done, pendetomy, complicated surgery.
So, we basically upgraded those facilities to reduce sending a patient to Warri, for three hours journey, instead take the service to them. In Ode-itsekiri PHC, they can do surgery there. In Irri PHC, by the time they start, they can do operations there. There will be a doctor. Infact, we are developing a new strategy now that we call if it is possible for a doctor to be at every PHC. If you go to PHCs it is either you see one old nurse and these people if they don’t see doctor, they don’t believe you. So we are planning to see if it will be possible to put a doctor in every PHC, even if it is not possible to put a doctor in every PHC, let there be a doctor in every ward because what we have right now is a doctor in every local government who is called the executive secretary but they are more of administrative.
They are not very much into clinical care but what we are saying is that as a minimum, let there be a doctor in a ward that will look after our PHC or a doctor in every PHC so that the people in the rural communities will feel the impact of healthcare properly.
Does The Scheme Covers Special Cases And When They Come Up How Do They Handle Such Cases?
First of all, we have a standard programme which we call our benefit package. Now there will be these special cases that will come up. It is there in our law, they can handle it but it is based on concession, it must be controlled. Two things activate the concessionary:
1. It should be an emergency. If it is an emergency, the hospital is allowed to do and let us know.
2. We must be aware. Because if it happens when we are not aware, we have to investigate or everybody will claim it. If you give us the records, we will go and investigate, find out what is going on and curb it but you see all these things have checks and balances. There is actually a fund domiciled in the Ministry of Health for intervention. It is called the special medical programme where if there is a peculiar situation.
It is kind of an assistance programme. If there is road traffic accident and government said treat them for free, it is from there but even in our health insurance scheme, we do that. I just finished investigating a case, somebody had a road traffic accident, was admitted in FMC, Asaba, stayed there, had treatment. He didn’t tell them that he had health insurance. It was when they gave him bills, he now brought out the card. They told him why didn’t you tell us, you wouldn’t have paid. It was then he started writing, but I have told them that if the case is genuine we will look at how to settle it.
If you have that peculiar challenge, you call us, there is a code we give to that hospital. It is called referral code. So that when the bills comes we will identify it because those things are now treated as special bill if not somebody can wake up one morning and say I received one man, no evidence. So, the evidence is that when the patient came you call us, you tell us the condition, we will look at it and confirm it and we will give you a code so that when you are submitting that bill, we identify it and pay and in between we will send somebody to go and confirm that. So, we take care of it but we must be notified and there must be a code associated with it.
Is There Anything Like Registration For Those In The Rural Areas Before They Benefit From This Health Insurance Scheme?
Those same people I am talking about, register everybody in the community, if you go to a house that have 50 people, you register all. Once there is under 5 and a woman that is pregnant, they are free, if there is a civil servant, it is free. So what we do we now identify those that don’t fall into the three categories. We have even made it easy for them that even if it is N100 that you have pay. There is a programme we are running in Warri, now, N100 daily.
If you pay N100 consistently for three months, you will be registered into the scheme. The fact that you are contributing that money shows that you are committed and in three months, you would have contributed half of the money, we register you into the scheme and allow you to pay the remaining.
Tell Us About The Formal And Informal Aspect Of The Scheme
In the law, there are three categories of enrollees. The first is the equity group, those are the ones we consider vulnerable (pregnant women, children under 5, elderly and physically and mentally challenged). The law also says that any organization that employs more than 10 people, falls into the formal sector. If there are 50 persons in a company and the highest person gets N200, 000, the least person is earning N30, 000 a month. If you collect from them individually, the one at the top will be enjoying while the one at the bottom will be suffering.
What we are saying is that do the total of what everybody earns, just pay 1. 75 percent of it, we will provide everybody free healthcare and it will cover you, your wife and four children. But if you are not in an employment that is when you pay N7, 000 a year , that is the informal sector. So, the difference between the formal and informal sector is how you pay not the service you receive. Everybody receives the same form of healthcare services. Every enrollee chooses the hospital that he or she wants. If they are not attending to you well in a hospital just write to us, you go to another hospital.
What Is Your Commission Doing About The Shortage Of Manpowers In Hospitals Across The State?
There is an embargo on employment, so there is nothing we can do but what we have intervened to do is the one of the reasons we said that we will pay money to the hospitals. Every hospital as I speak with you can actually employ a ad-hoc nurse and they will pay from the hospital, the only thing is that those people cannot be in the payroll, that is the only difference. There was a time the governor gave a directive that they should employ two nurses, two community health extension workers’ but it must be on ad-hoc basis.
But he also gave a directive that the people employed must be people resident in the community and I can tell you now that the governor has approved for the employment of 40 pharmacists, all the hospitals adhocs during the Covid-19, they have all been employed into Delta state officially. We are equipping the nurses to run the hospitals as a business entity. You work, you earn money, you benefit from it.
As A Commission, What Are Some Of Your Challenges?
Our challenge is the fact that there is a lot of mistrust in government policies. People don’t just trust government, it is a big issue. I never forget one experience that I had. When I started this programme, civil servants mistook the contributory health not knowing that there was contributory pensions.
So we started educating them between the two, they didn’t listen. We pride ourselves with the fact that there is that ability to show that the health insurance scheme works. It is an evidence based activities that we do. So, the biggest challenge that we have is convincing people that there is a possibility that this thing will be truthful. The next challenge is getting our healthcare workers to change their mindsets, they are used to get to work at 10:00am, close by 4:00pm. No, it has changed, you must come to work on the morning, close in the evening. Another challenge is that we need their mentality to change because before in our early days, the nurse or health worker was a king but the thing has changed, the customer is the king. Why?
Because you have collected that person’s money upfront. So, changing that mentality of our healthcare providers where they think they are the king is very important, because customers are now kings. You must respect, treat them well because without the customer, you won’t be in employment. So, those are the challenges we are having, most of the other ones are things we can surmount, they are typical basic challenges. If we are able to change peoples’ mindsets and get our healthcare providers to change their orientation, 50 percent of our challenges would have been solved.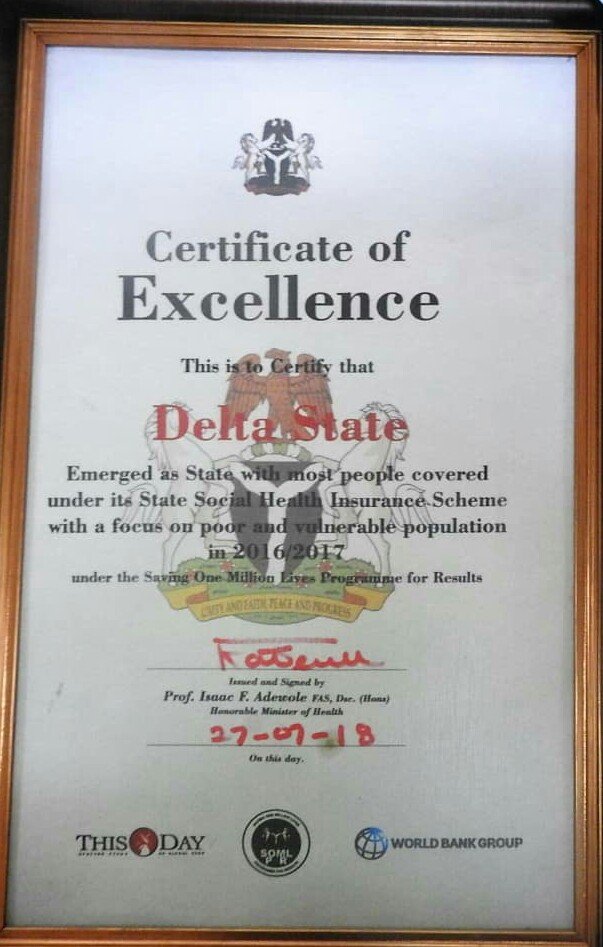
What Would You Like To Be Remembered For As The Pioneer Director General Of The Delta State Contributory Health Commission When You Finally Leave Office?
The most important thing that, I want to be remembered for is that I had an opportunity to make healthcare service available to all residents of Delta state particularly those in the very rural communities that has not had access to healthcare for a very long time, that is my dream. The reason is that it is a passion for me, since I graduated as a doctor, this is what I have been doing. Two, is that I also want a situation where when I leave, there is an established organization running here.
That is why the first thing I did when I came on board, I went to the governor and said all the workers that are going to work here they are all going to be empowered to be able to run the organization and because I am going to put them through the out of normal, I requested for a special duty allowance. Every staff from head to bottom gets a special duty allowance for working here and the money is not small. Three, is we do training, there is nobody in this office that is not ICT compliance. Also, is the fact that I want a situation where we are always an example for the country and we always want to set the standard. Why? Is because our governor is a champion for healthcare and health insurance.
So we have to be always be on top of our game to make sure we portray the state very well. The only part that gets me worried and emotional is when there is this negative castigation based on false information. There must be a balance, when issues come up, we are open, call us and we will explain to you.